One of the biggest hurdles to treating tongue tie or upper lip tie is the comfort level of the practitioner, especially if they do not perform a large volume of procedures. An additional obstacle is that the professionals who are capable of treating babies (ENTs, pediatricians, oral surgeons, family practitioners, midwives and nurse practitioners) all have varied training backgrounds. This makes a consistent approach to treating tongue tie and lip tie difficult to achieve. As a result, most practitioners simply practice what they were taught instead of looking for alternative options.
Mothers around the world have related to me frustrating scenarios like this:
- Baby and/or mom have breastfeeding symptoms related to tongue or lip restriction
- Their doctor or lactation consultant correctly identifies tongue tie or lip tie and refers them to an ENT or oral surgeon
- The surgeon is not comfortable doing the procedure in the office and requires general anesthesia (GA)
- The anesthesiologist is not comfortable doing "elective" procedures on babies until they are 3 (and often 6) months of age
- While baby waits, mom and baby can't keep breastfeeding and the relationship is lost
Before explaining how to perform frenotomies in the office, I want to briefly review why general anesthesia should be avoided if possible. The first reason GA should be avoided has to do with the potential effects on children. There are numerous animal studies that have shown that inhalational anesthetics in addition to injected anesthetics like ketamine and propofol are neurotoxic. They cause nerve cell death in developing animals. There are several retrospective human studies that have shown potential problems. One of the most publicized studies from the Mayo Clinic in 2012 showed: "Children repeatedly exposed to procedures requiring general anesthesia before age 2 years are at increased risk for the later development of ADHD." While prospective studies are still in progress, I feel that there is enough evidence showing that GA can affect children, and if there's an alternative to using GA, it should be pursued. There are also obvious inherent immediate risks to GA - reactions to the anesthetics which can lead to other health problems. There is nothing safer than completing avoiding it if possible.
Secondly, the baby is away from mom and nursing after emerging from anesthesia isn't a fluid process. The baby must wake up in the recovery room, often connected to monitors, and getting mom back to the room to nurse isn't always easy. The effects of the anesthetic, even in short cases, can linger throughout the day and disrupt normal breastfeeding routines.
Finally, it's a cost. Because these babies are young, the procedure is almost always done in a hospital instead of an outpatient surgery center. There are two fees incurred when you choose GA: the anesthesiologist's fee and the hospital facility fee. By far, the facility fee is much higher, and in situations where families are already paying for the birth of their child, this can be cost prohibitive.
By far, the most common reason that is cited by those who wish to avoid performing in-office frenotomies is the fear of uncontrolled bleeding. This potential complication can be mitigated by proper training. Between April 2012 and April 2013 (prior to my use of laser), I performed 203 tongue and lip procedures with scissors in the office on children up to 12 months of age. None needed cautery or stitches. What is my basic protocol for performing tongue and lip-tie revision with scissors?
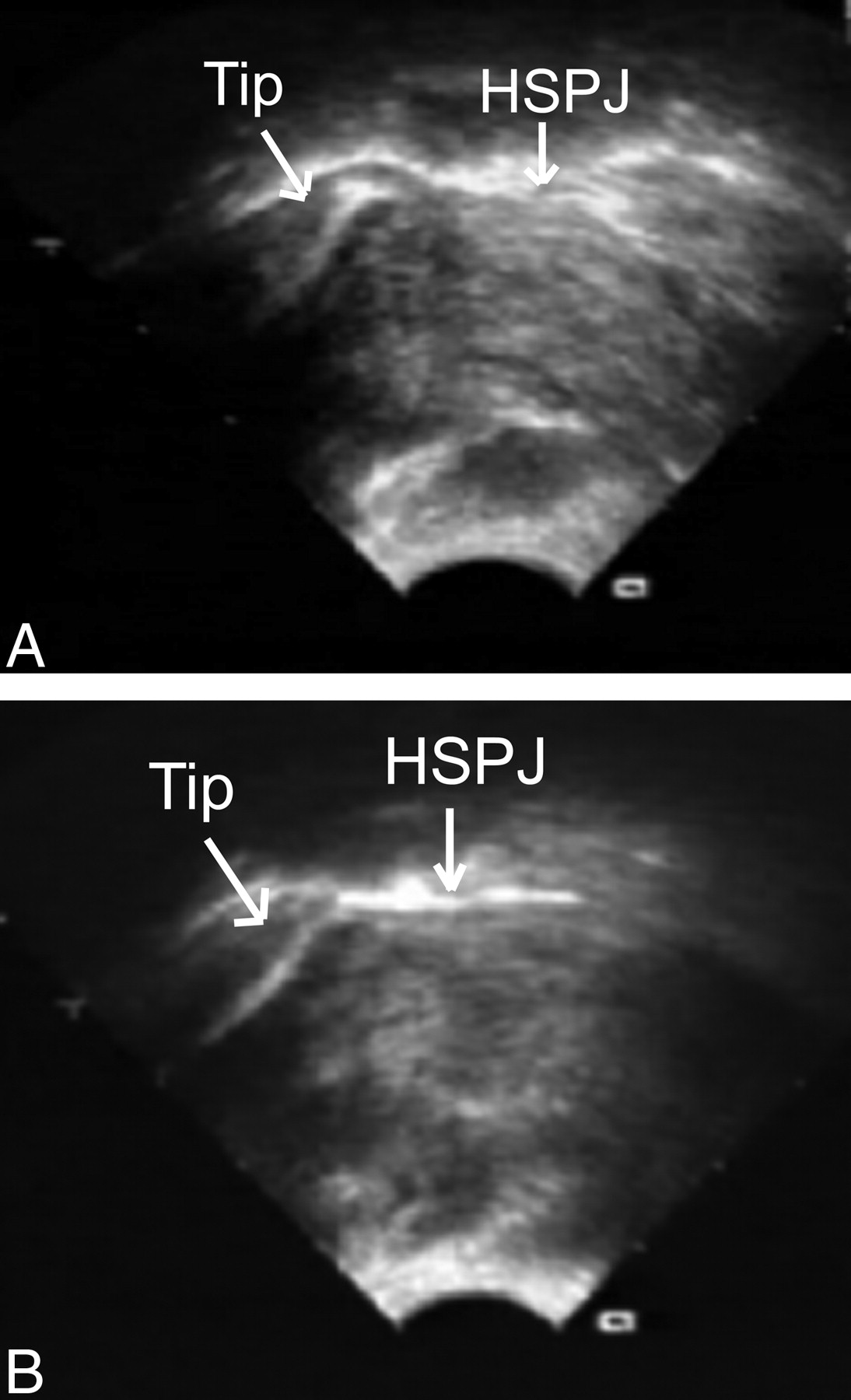
- I have all equipment ready for the procedure ahead of time: tenotomy scissors, a grooved director, gauze, a topical numbing cream with Q-tips (I use EMLA as benzocaine is now contraindicated in children under 2 years of age), an injectable anesthetic (1% lidocaine with 1:100000 epinephrine using a 30g needle), and gauze floating in ice cold water.
These instruments come in various sizes - I prefer the 6" long rather than the 4" long versions. Left - a grooved director for isolating the tongue tie. Right - tenotomy scissors.
- The baby is swaddled on a flat table with an assistant stabilizing the head (alternatively a parent or another assistant can restrain the arms. The upper lip tie (if it will be treated) is swabbed with EMLA. 30 seconds later, I inject a small amount of the injectable anesthetic into the lip tie (especially along the gumline). I then wait 10 minutes for the epinephrine to cause vasoconstriction. This same technique can be utilized for the posterior component of the tongue tie, although I do not feel it to be necessary. I typically use EMLA on the tongue tie right before the procedure.
- After 10 minutes, I either simply snip the lip tie by hugging the gumline or completely excise the lip tie with several small cuts. I find that the excision of the lip tie (a frenectomy) results in fewer babies with reattachment of the wound. The key is pulling up on the lip with a gauze pad to prevent it from slipping. Adequate tension on the wound minimizes bleeding.
- Once the lip tie is treated, a grooved director is inserted to isolate the lingual frenulum and a cut is made to go completely through the posterior component. A light finger sweep should confirm that no residual band exists. The result should be a diamond-shaped wound. If there's no diamond shape, there is more tie to be cut.
- Pressure is held on the wound with cold gauze until mom is ready to nurse, and then baby goes directly on the breast (or bottle). Within seconds to minutes, the bleeding stops.
This technique results in effective release of tethered bands and can significantly improve breastfeeding outcomes without the use of general anesthesia. Despite all this, if a mom's only option is to go to a provider who uses GA, then I most certainly recommend it. In my opinion, the benefits of prolonging the breastfeeding relationship far outweighs the risks of GA. However, if you have a provider who is receptive to doing tongue and lip-tie revision without general anesthesia, please feel free to have them email me and I can help to facilitate these simple in-office procedures.